The ACT-Accelerator has supported the most rapid and coordinated effort in world history to develop tools to fight disease.
How the the ACT-Accelerator works
The Access to COVID-19 Tools (ACT) Accelerator is a time-limited global collaboration designed to rapidly use existing global public health infrastructure and expertise to accelerate the rollout of COVID-19 diagnostic tests, treatments and vaccines globally and overcome inequities in low- and middle-income countries.
What does the ACT-Accelerator do?
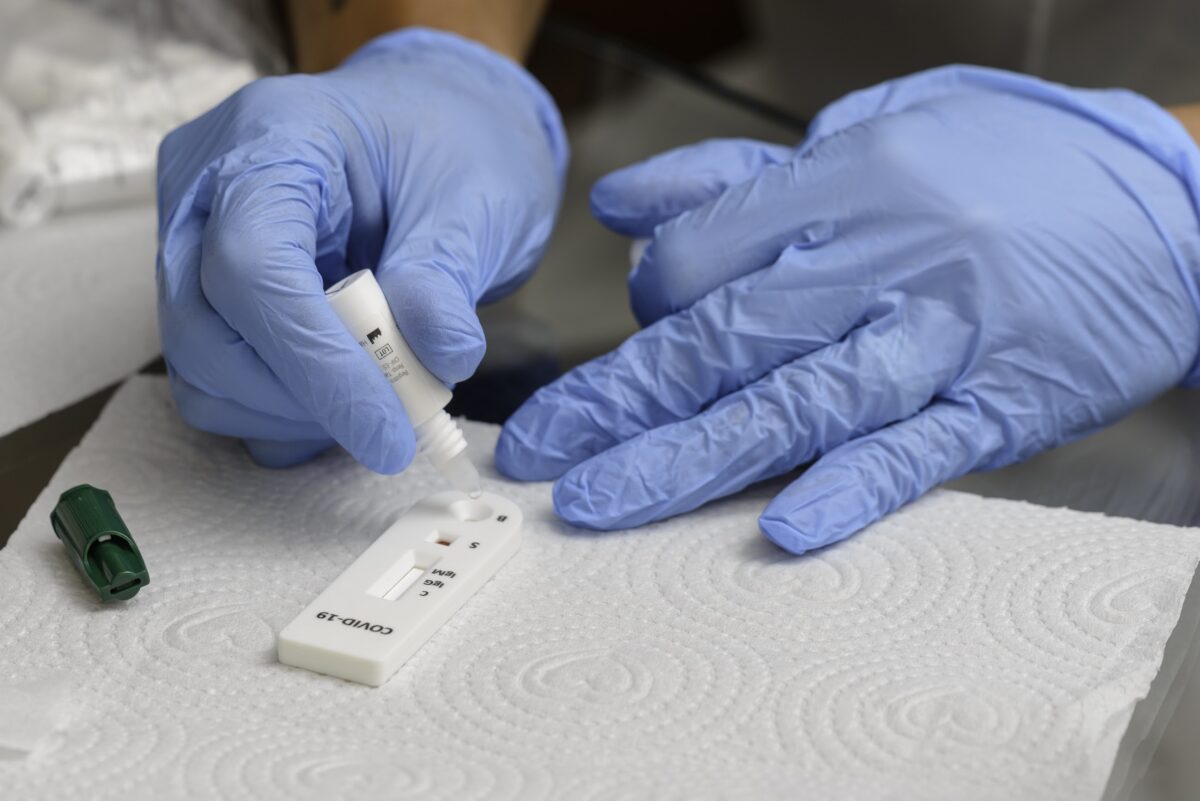
The ACT-Accelerator focuses on development, production and equitable access to COVID-19 tests, treatments and vaccines.
Launched in April 2020, it has supported the most rapid and coordinated effort in world history to develop tools to fight disease.
Now, ACT-Accelerator is expanding to provide access to COVID-19 tools globally.
Who is involved?
The ACT-Accelerator brings together expertise from several global health institutions, academic researchers, policymakers, regulators, the private sector, including research and development, the manufacturing industry, and those working on market shaping, procurement and delivery.
How does it work?
The ACT-Accelerator focuses on vaccination, diagnostics and treatment.
The Diagnostics Pillar is co-convened by the FIND, the global alliance for diagnostics (FIND) and the Global Fund, focusing on the needs of low- and middle-income countries in their fight against COVID-19.
World partners
WHO leads programmes on regulatory policy, product procurement, allocation, and country access and support. The organization also supports research and development.
The Health Systems Connector (HSC) works across the three product pillars. It is co-convened by the Global Fund, the World Bank, and WHO, with support from The Global Financing Facility for Women, Children, and Adolescents (GFF).
What are the ACT-Accelerator’s goals?
To identify and address country-specific issues that delay the rollout of tests, vaccines or treatments and ensure that there is sufficient personal protective equipment (PPE) available to health workers.