India’s digital ecosystem for COVID-19 management has centred around Aarogya Setu – Sanskrit for “Bridge to Health” – a public-facing mobile application designed in response to the pandemic.
Software engineers, epidemiologists, statisticians, social scientists and legal experts from across India started to work with the Indian government to develop a digital response to the pandemic in March 2020.
The resulting systems, new digital tools as well as adapted existing tools, aimed to help test-trace-isolate (TTI) programme activities, predict emerging hotspots and identify high-risk individuals in need of targeted testing.
This case study examines how India leveraged these digital solutions in their COVID-19 response.
India’s numbers
First confirmed COVID-19 case: 28 January 2020.
1 March 2021: 11-million cumulative cases detected from 227-million tests.
15 March 2021: 2,19,262 active cases, a cumulative recovery rate of 96.7% and death rate of 1.4%.
The digital backbone of Aarogya Setu
Aarogya Setu, the backbone of India’s COVID-19 management strategy, is a mobile application launched on 2 April 2020. By November 2020, it had 170 million registered users, or 13% of the country’s population.
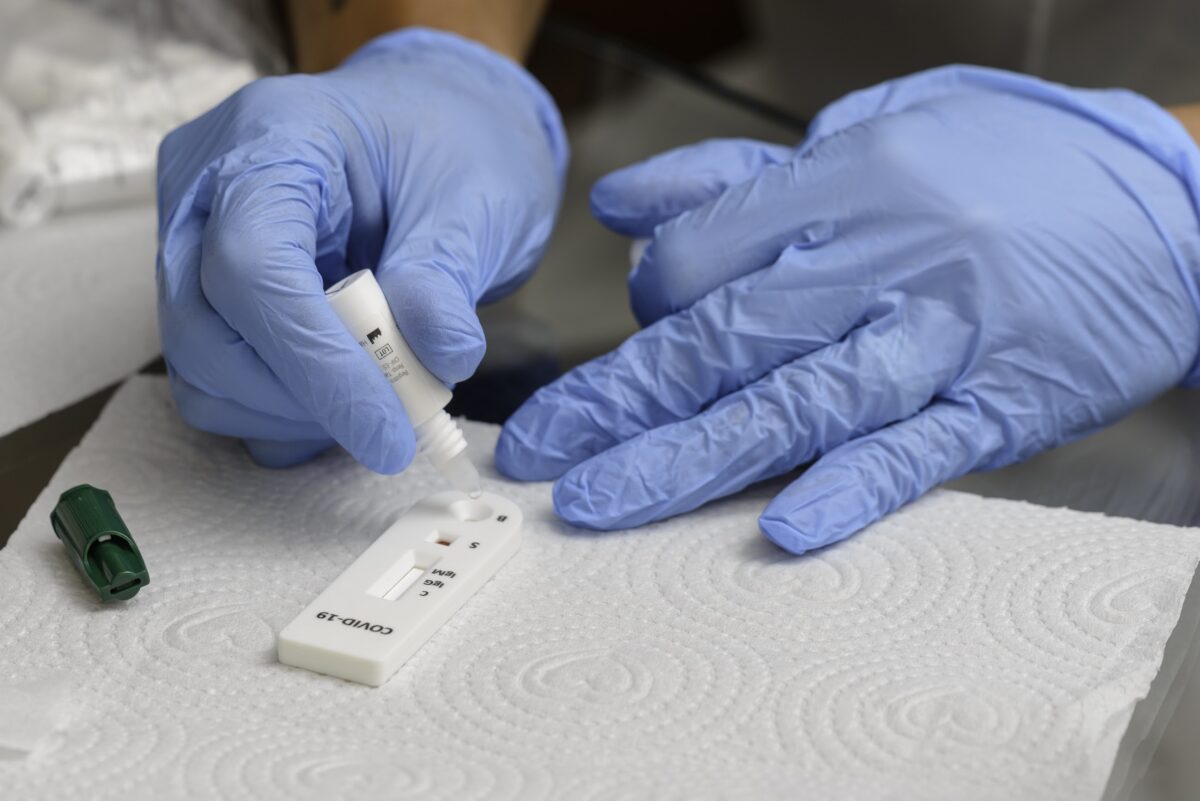
Users download the app free and register using their mobile number, following which a de-identified identification (DID) is generated to enable anonymised transfer of their data in the system. It captures two key sets of data:
- Self-reported symptoms – for case management and hotspot mapping
- Location (via Bluetooth) for contact alerts
Aarogya Setu then scores user risk based on exposure to confirmed cases to determine who is at high risk of infection and should be prioritised for testing. Based on this, follow-up actions are recommended: Caution, Quarantine or Test.
Information on high-risk individuals is also transmitted to the Ayushman Bharat call centre, which follows up with them by phone to support linkage to testing and care.
Within the first eight weeks of the app’s introduction, more than 900 000 users identified through the algorithm had been contacted.
India’s response also leveraged the pre-existing electronic infrastructure of Ayushman Bharat, the National Health Authority (NHA) scheme to provide free healthcare to 500-million citizens.
The IT-enabled Integrated Hotspot Analysis System (ITIHAS) uses syndromic data submitted by Aarogya Setu users to map future hotspots. This in turn informs targeted testing strategies.
ITIHAS also generates hotspot predictions using the historic location data, based on cell phone tower signals, of confirmed positives diagnosed in the Indian Council of Medical Research (ICMR)’s network of approved labs.
Digital tools: the benefits
Digital health solutions can help address high-priority gaps, particularly in India, which has high overall digital maturity and a rapidly evolving digital health landscape.
Digital solutions tailored to support the integration and/or bundling of tests provide an opportunity to identify at-risk patients earlier and intervene faster.
Practical ways to scale
India’s government has established a positive and enabling environment for ICT intervention in health.
In August 2020 the country launched the National Digital Health Mission, in which every Indian was due to receive an electronic health account in the form of a mobile application.
Challenges
Despite its digital maturity, India’s health system is underfunded, with government healthcare spending only 0.96% of its GDP.
This is lower than spend in other low- and middle-income countries (1.3%), and BRIC countries (3.0%). It contributes to a lack of adequate public health services, especially in rural areas.
India’s population relies heavily on private health providers, in the face of an under-resourced and unregulated health system, skilled staff shortages and disparate management systems.
KEY INSIGHTS
India has an increasingly low-cost and fast digital infrastructure, with high mobile phone penetration and growing smartphone penetration. This has enabled extensive use of the Aarogya Setu mobile app.
As mobile penetration and ICT literacy in India is growing rapidly, scale-up of digital health tools will be necessary to optimise the nation’s limited resources, bridge inequity in healthcare access and strengthen the availability of quality diagnostics.