Rwanda has raised the bar in using digital tools to scale up community-based testing in its COVID-19 response.
A national Joint COVID Task Force, established in February 2020 before the first case was confirmed, led the pandemic response of this African country. The team gave both high-level strategic guidance and day-to-day operational support.
This had, however, been preceded by years of investment in the broader digital health infrastructure, where digital technologies were expanded to support service delivery – a longstanding government priority.
Institutions in Rwanda were therefore able to combine resources and capacities to respond to emerging problems. Adopting a multi-sectoral approach from the start has allowed rapid deployment of interventions and more efficient troubleshooting.
It also helped the country to build COVID-specific digital systems to strengthen the areas of testing, contact tracing, patient support and surveillance.
Rwanda’s numbers
First registered COVID-19 case: 14 March 2020
14 March 2021: more than 20 000 cases diagnosed, with mortality rate of 1.4%
Sharpest peak in cases: late 2020 and early 2021. This prompted stringent restrictions on movement that led to a rapid decline in new cases.
Testing the toolbox
Rwanda has used District Health Information Software (DHIS-2) to survey and monitor disease since 2011 and, in early 2020, this system was adapted to capture data on COVID-19 diagnosis and case management.
DHIS-2 is integrated with the laboratory information system which allows for automated transmission of data.
COVID-19 Command Posts, the sub-national operational centres of the Joint COVID Task Force, receive and analyse surveillance data from these different systems to inform policy and programme decisions.
Rwanda also devised a stringent port of entry system to avoid importing COVID-19 cases.
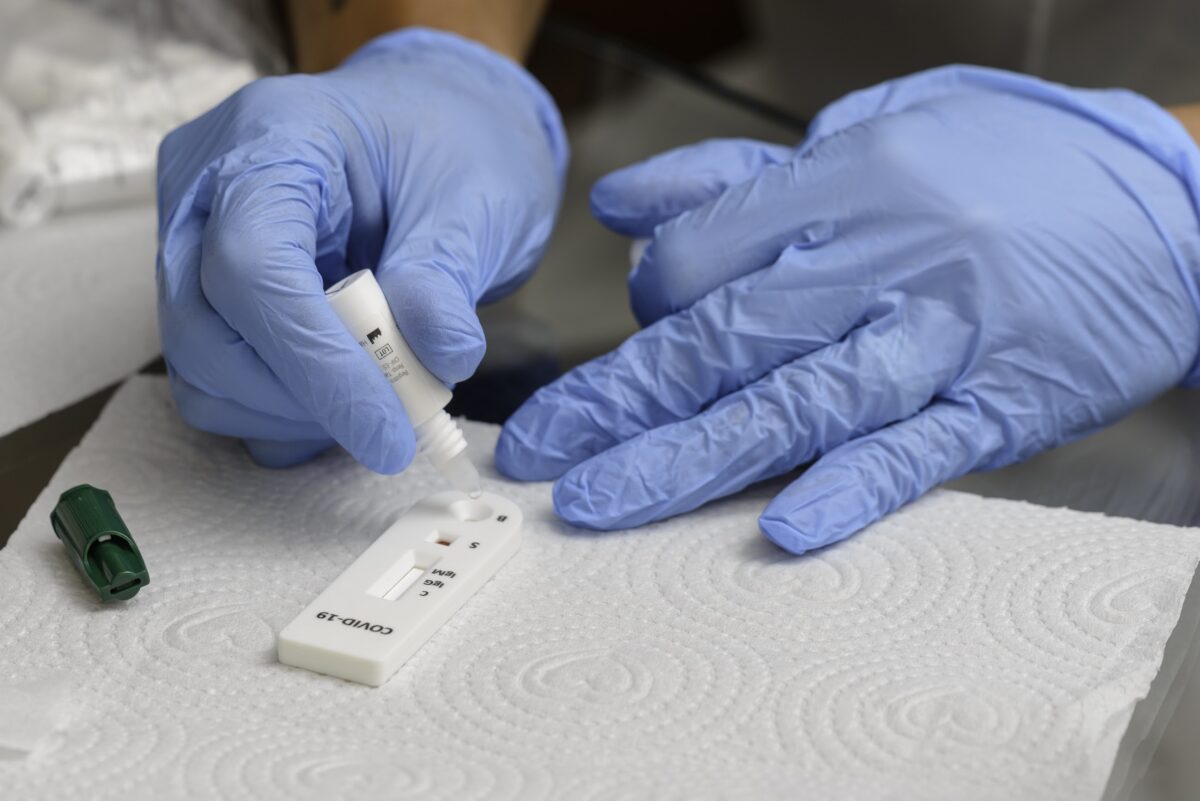
Other technologies were deployed in selected settings, including the internal Visitor Tracking Record and the e-ASCOV pilot, a locally developed application to help give access to rapid antigen testing.
Patient-facing tools
- WhatsApp help line
- Unstructured supplementary service data (USSD) platform, which provides basic information on COVID-19 on any phone with no data or airtime requirements
- WelTel app, where patients can report symptoms
- Standard electronic medical record (EMR) system
- Online results portal
- Open Data Kit (ODK) application which captures data for targeted surveillance activities outside of health facilities, particularly in hotspots.
Impact of digital tools
The use of digital tools in Rwanda has had a significant impact. For example, through integrating laboratory and health management information systems, the testing process is now paperless. All facilities capture data in the same central system.
Patient unique health codes (UHCs) also allow data transfer between different digital solutions. This cuts down the time taken by health care workers to record and report data, as it is captured in real-time at the point of care.
Application programming interfaces have also been developed for a number of tools to enable interoperability.
Mobile-data collection tools for community-based surveillance have generated valuable insights to inform timely responses to outbreaks.
Monitoring cases and contacts remotely using digital tools has reduced the burden on the health system. This has allowed the country to focus limited capacity on delivering services to the most at-risk individuals, while consistently monitoring other patients.
Key success factors in Rwanda
- Pre-existing digital infrastructure
- Political will, with digital infrastructure bolstered by political commitment at the highest levels of government
- National ownership of systems, minimising the challenge of isolated pilots, duplicate interventions and “data fog”
- Building on existing tools
- Multisectoral collaboration
- Providing patients with direct access to results.
Challenges
The lack of readiness of health care workers to adopt new digital tools can be a barrier to successful implementation.
This is worsened in a crisis such as COVID-19, where systems are already overwhelmed with new protocols and interventions.
Resource requirements are also unpredictable due to the rapidly evolving nature of the pandemic.
It is important to coordinate decisions on selection of digital tools from among numerous vendors.
KEY INSIGHTS
- Ensuring integration of national COVID-19 data (public and private sector) into one platform enhances understanding of the pandemic and simplifies data management.
- Leveraging databases in other areas can minimise the time and effort required for individual data capture.
- Digital tools, particularly on mobile devices, are key in providing decentralised testing services.
While Rwanda is still in the early stages of rolling out its approach, it shows potential to expand and standardise testing outside of health facilities.